Entry Version:
Citation:
Pancreapedia: Exocrine Pancreas Knowledge Base, DOI: 10.3998/panc.2015.39
| Attachment | Size |
|---|---|
| 235.48 KB |
1. Introduction
Acute pancreatitis (AP) is a common clinical condition with a significant morbidity and mortality. AP has many causes and can be multifactorial. The role of genetic factors appears to be complex and is expanding as genetic mutations and their interactions with environmental influences undergo further investigation. If not corrected, any factor responsible for pancreatitis is capable of producing relapsing pancreatitis and hence it is important to carefully evaluate the patient and address the underlying issue.
The problem is compounded because multiple etiologies are present in at least 7% of patients, especially genetic predispositions plus another factor (toxic or obstructive). Establishment of the etiology of acute pancreatitis often requires expensive and sometimes invasive evaluation, some of which entails risk for significant complications, including further pancreatitis.
2. From AP to CP
Increasingly, it is understood that a continuum exists between recurrent AP and chronic pancreatitis (CP). When thoroughly investigated with newer sensitive techniques such as secretin-enhanced magnetic retrograde cholangiopancreatography (S-MRCP), endoscopic ultrasound (EUS), and pancreatic function tests, many patients presenting with isolated recurrent acute episodes of pancreatitis and a minority of those presenting with their first acute attack are found to have morphologic evidence of CP, ranging from subtle “minimal change” disease to obvious disease with calcifications. Over time, some patients with AP and apparently normal morphology progress to obvious CP with calcifications and loss of endocrine and exocrine function (6, 11, 12). The exact mechanism by which acute pancreatitis progresses to chronic pancreatitis is not well understood.
It is not clear if a sentinel event starts an inflammatory process that cannot be turned off (sentinel AP event = SAPE hypothesis) or if the pathology simply represents accumulated damage from prior attacks that has not fully healed. It remains to be established why some patients after either a single or a few attacks of AP have an aggressive disabling course leading to CP with permanent structural changes of the gland, chronic abdominal pain and exocrine and endocrine dysfunction, whereas others have a harmless course without development of fibrosis or dysfunction. The etiology of AP is thought to have an influence on the course of the disease, since previous studies indicate that a major part of alcohol-induced AP seems to progress to CP, whereas this is only rarely the case for biliary-induced AP. Necrotizing AP, however, can lead to pancreatic insufficiency and permanent ductal lesions (10). Exocrine and endocrine functional impairment has been described even after mild non-alcoholic AP (9). In patients with acute recurrent pancreatitis and CP, a disconnect between symptoms and morphology is often seen, such that patients with obvious CP by morphology may have minimal chronic symptoms between attacks of AP, whereas those with a normal-appearing pancreas between acute relapsing pancreatitis attacks may suffer intractable chronic pain. In these patients, it is not clear if pain is from low-level chronic inflammation or if it has a functional cause unrelated to the pancreatitis. Data are limited on the natural history of acute pancreatitis. In one study evaluating the natural history after the first attack of AP, recurrent pancreatitis was seen in up to 16.5% of the patients at a mean follow-up of 7.8 years (5).
The annual relapse rates were higher for those with alcohol and gallstones as an etiology and about 1% per year or less for other etiologies, including those termed “idiopathic”. Recurrence rates in other studies of recurrent pancreatitis have been seen up to 3-4 times this rate over 2-3 years. Genetic mutations are thought to play a significant role in the recurrence of pancreatitis or perhaps play a significant role in the disease progression and may serve as a cofactor (multi-hit hypothesis). Various genetic mutations have been recognized as a cause. The interplay between genetics and environmental risk factors is not well understood. The utility of routine clinical testing for genetic mutations is unclear (8).
Several interventions are offered for management of acute recurrent pancreatitis. There are limited data to support the role of minor papillotomy for those with pancreas divisum and recurrent acute pancreatitis. Long term data are lacking. Similary the role of sphincter of oddi dysfunction as a cause of recurrent acute pancreatitis is very controversial. When manometry is performed and endosphincterotomy is performed, addition of pancreatic sphincterotomy to biliary sphincterotomy has provided no additional benefit (2).
One should be careful in offering endoscopic therapies for these entities and when done should be done in a setting of a carefully planned research study. Measurement of treatment success in a disease where multiple factors play a role is difficult and defining the end-points is difficult as well. There is also a concern of further damage to the pancreas by interventions such as post ERCP pancreatitis, stent induced strictures in the pancreatic duct even when stents are placed for a short term for prevention of post ERCP pancreatitis (1). When endoscopic procedures such as ERCP for possible sphincter of Oddi dysfunction or pancreas divisum are done one should weigh the risk of complications of the procedures carefully. These procedures are best done in a setting of clinical research. In a disease with a natural history and where there is a significant interplay with other co-factors determining the end points of therapy and measurements of outcomes are difficult (7).
3. Mortality and Risk Factors for Progression to CP
In a Danish prospective study of 352 patients with AP and a 30-year complete follow-up by the Danish registries, 24.1% of the patients with a first attack of AP progressed to CP (progressive acute pancreatitis). CP was diagnosed a mean of 3.5 years after first admission for AP. The mortality in patients with progressive acute pancreatitis was 2.7 times higher than the mortality in patients that did not progress to chronic pancreatitis, and compared with the background population the mortality was 5.3-6.5 times higher. The risk of progression decreased with increasing age and in a Cox regression analysis with age included as a co-factor, smoking was the most important factor associated with progression from AP to CP while gallstone-induced AP showed a trend towards significance. Gender and employment showed non-proportionality. Alcohol had no significant influence on the progression (6, 13).
4. Conclusions
Recurrent AP is a common clinical condition. After confirming the attacks are truly pancreatitis, the etiology is apparent in at least 70% to 80% of cases with simple investigations. Another 10% to 15% can be found with more advanced testing, and up to 10% are idiopathic. However, certain etiologies identified by these tests are not universally agreed upon as being important or relevant. The role of empiric cholecystectomy is unclear. Genetic predisposition is a common cofactor, but the role of routine testing is still unclear, except in those with a family history and suspected PRSS1 mutation (which identifies a higher cancer risk). Evolving research in medical therapy of patients with CFTR mutation may change this, and expand the role of genetic testing. The natural history of the disease and the treatment effects are poorly understood. It is a syndrome of various causes, symptoms and outcomes. Longer term follow-up and well-designed, preferably randomized, studies with adequate sample size are needed. Invasive procedures, especially ERCP, solely for diagnostic purpose (without manometry or divisum-targeted therapy) should be avoided. MRCP and EUS are recommended after a complete history and physical, routine laboratory tests including evaluation of triglycerides, and imaging studies, especially in recurrent disease: EUS is preferred in older patients and in those with gallbladder in place, because of its superior performance for small tumors and subtle gallbladder lithiasis (small stones or sludge in the gallbladder).
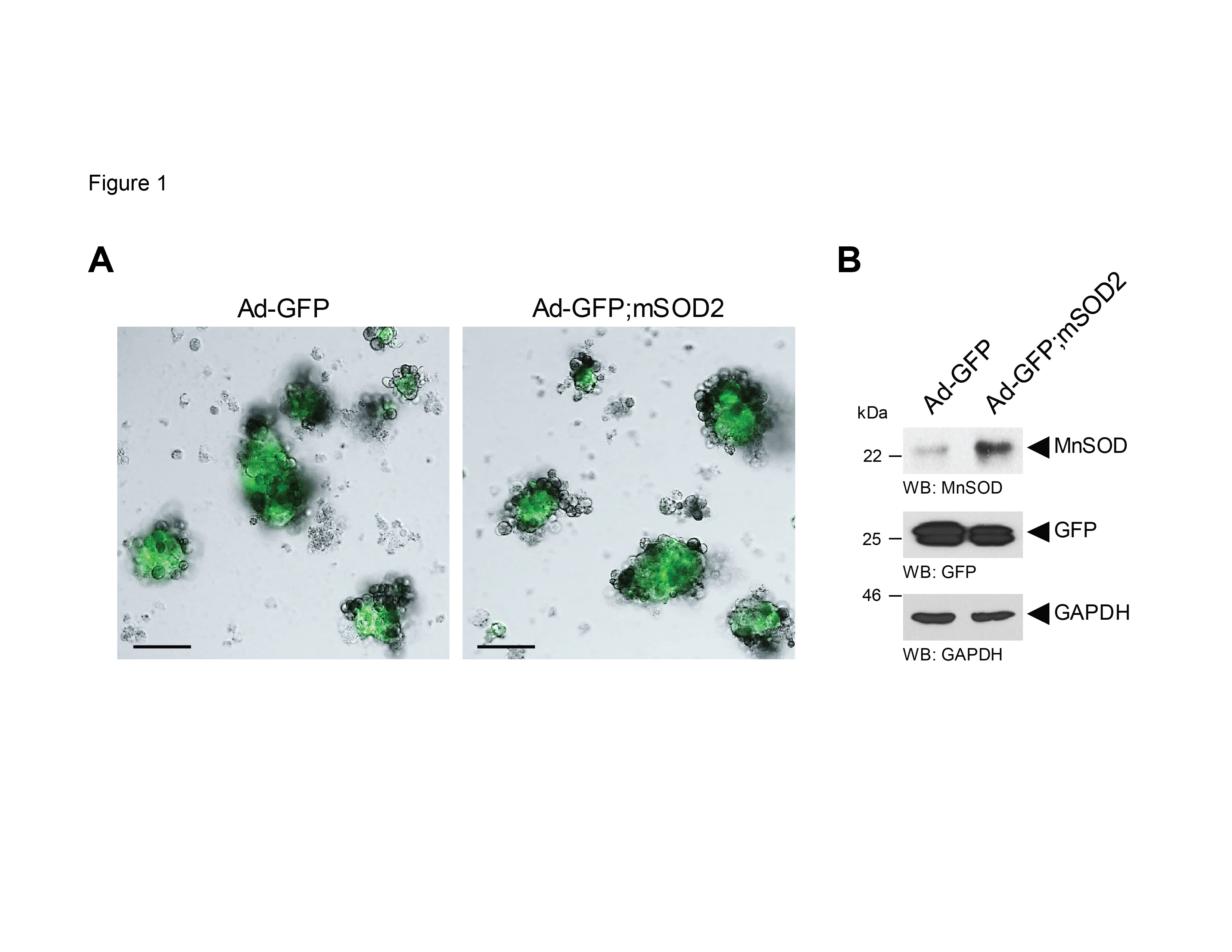
Figure 1. EUS image of a patient with idiopathic acute recurrent pancreatitis. No calcifications were seen but the gland shows lobularity and honey combing features which are suggestive but not definitive of chronic pancreatitis.
Establishing subtle evidence of chronic pancreatitis may be worthwhile in patients with intractable pain between attacks, and the role of aggressive resection in recurrent acute pancreatitis without CP is evolving. One should not rely on morphological features alone to diagnose chronic pancreatitis. A classification based on a combination of morphological examinations, exocrine pancreatic function tests and imaging procedures is recommended (5).
AP can progress to CP (Figure 1) and smoking is the strongest risk factor associated with progression. The mortality is 5-6 times higher compared with the background population, indicating that patients with AP and risk factors for CP should be followed. As the disease is multifaceted, treatment for smoking dependency, alcohol dependency, and nutritional support is encouraged. Endoscopic investigations and therapy should be carefully weighed against the risks and should preferably done in expert centers. There are no definite guidelines or consensus regarding the clinical follow up for patients with recurrent acute pancreatitis. There is consensus that these patients should avoid smoking to reduce the risk of progression of the disease. Any other triggering risk factor should be carefully avoided including cessation of alcohol or any suspected medicine. Triglycerides should be checked. Clinical follow up with further investigations based on clinical symptoms is appropriate. There are no data to support routine periodic surveillance with invasive procedures such as EUS or to carry out routine CT scans since there is a significant risk of radiation exposure. There are currently no biomarkers available to monitor disease progression. If one should develop a recurrent episode once the acute episode is managed, further investigations as appropriate should be done. It might not be unreasonable to repeat endoscopic ultrasound or in appropriate circumstances offer other endoscopic/surgical interventions (Figure 2).
Figure 2. Algorithm for approaching patients with recurrent acute pancreatitis. Work up on the left with less risky interventions have more proven benefit of intervention than those on the right (red boxes). Adapted from (4).
5. References
- Bakman YG, Safdar K and Freeman ML. Significant clinical implications of prophylactic pancreatic stent placement in previously normal pancreatic ducts. Endoscopy 41(12): 1095-1098, 2009. PMID: 19904701.
- Cote GA, Imperiale TF, Schmidt SE, Fogel E, Lehman G, McHenry L, et al. Similar efficacies of biliary, with or without pancreatic, sphincterotomy in treatment of idiopathic recurrent acute pancreatitis. Gastroenterology 143(6): 1502-1509 e1501, 2012. PMID: 22982183.
- Etemad B and Whitcomb DC. Chronic pancreatitis: diagnosis, classification, and new genetic developments. Gastroenterology 120(3): 682-707, 2001. PMID: 11179244.
- Guda NM, Romagnuolo J and Freeman ML. Recurrent and relapsing pancreatitis. Curr Gastroenterol Rep 13(2): 140-149, 2011. PMID: 21286872.
- Lankisch PG, Breuer N, Bruns A, Weber-Dany B, Lowenfels AB and Maisonneuve P. Natural history of acute pancreatitis: a long-term population-based study. Am J Gastroenterol 104(11): 2797-2805; quiz 2806, 2009. PMID: 19603011.
- Nojgaard C, Becker U, Matzen P, Andersen JR, Holst C and Bendtsen F. Progression from acute to chronic pancreatitis: prognostic factors, mortality, and natural course. Pancreas 40(8): 1195-1200, 2011. PMID: 21926938.
- Romagnuolo J, Guda N, Freeman M and Durkalski V. Preferred designs, outcomes, and analysis strategies for treatment trials in idiopathic recurrent acute pancreatitis. Gastrointest Endosc 68(5): 966-974, 2008. PMID: 18725158.
- Shelton CA and Whitcomb DC. Genetics and treatment options for recurrent acute and chronic pancreatitis. Curr Treat Options Gastroenterol 12(3): 359-371, 2014. PMID: 24954874.
- Symersky T, van Hoorn B and Masclee AA. The outcome of a long-term follow-up of pancreatic function after recovery from acute pancreatitis. JOP 7(5): 447-453, 2006. PMID: 16998241.
- Tsiotos GG, Luque-de Leon E and Sarr MG. Long-term outcome of necrotizing pancreatitis treated by necrosectomy. Br J Surg 85(12): 1650-1653, 1998. PMID: 9876068.
- Umapathy C, Raina A, Saligram S, Papachristou GI, Rabinovitz M, Chennat J, et al. 591b Natural History After Acute Necrotizing Pancreatitis (NP): A Large U.S. Tertiary Care Experience. Gastroenterology 148(4): S-113-S-114.
- Yadav D, O'Connell M and Papachristou GI. Natural history following the first attack of acute pancreatitis. Am J Gastroenterol 107(7): 1096-1103, 2012. PMID: 22613906.
- Yadav D, Slivka A, Sherman S, Hawes RH, Anderson MA, Burton FR, et al. Smoking is underrecognized as a risk factor for chronic pancreatitis. Pancreatology 10(6): 713-719, 2010. PMID: 21242712.